If you’re pregnant or postpartum and researching diastasis recti, you’ve probably encountered conflicting advice. Some sources say never do Pilates with DR. Others claim certain exercises will “close your gap.” The truth is more nuanced, and understanding it will help you make informed decisions about your body and your recovery. Let’s cut through the confusion with actual evidence and practical guidance.
What Diastasis Recti Actually Is
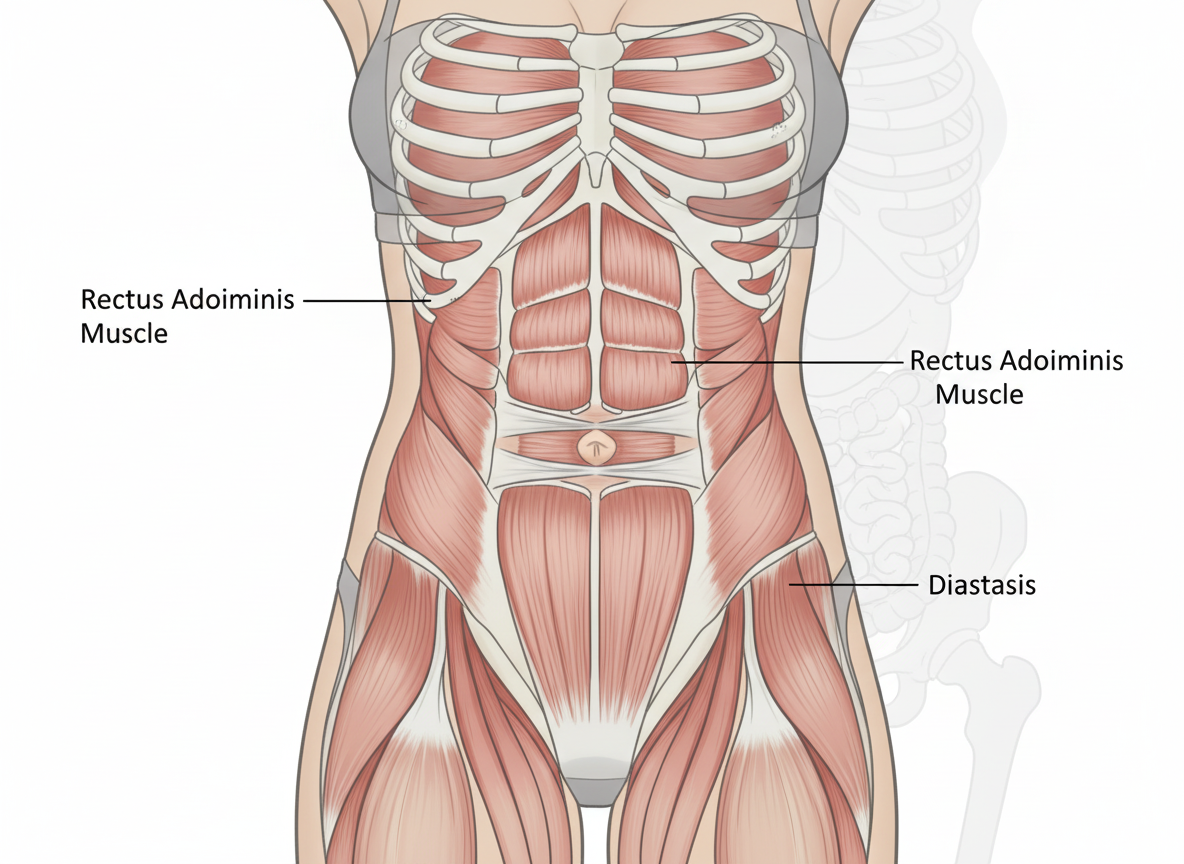
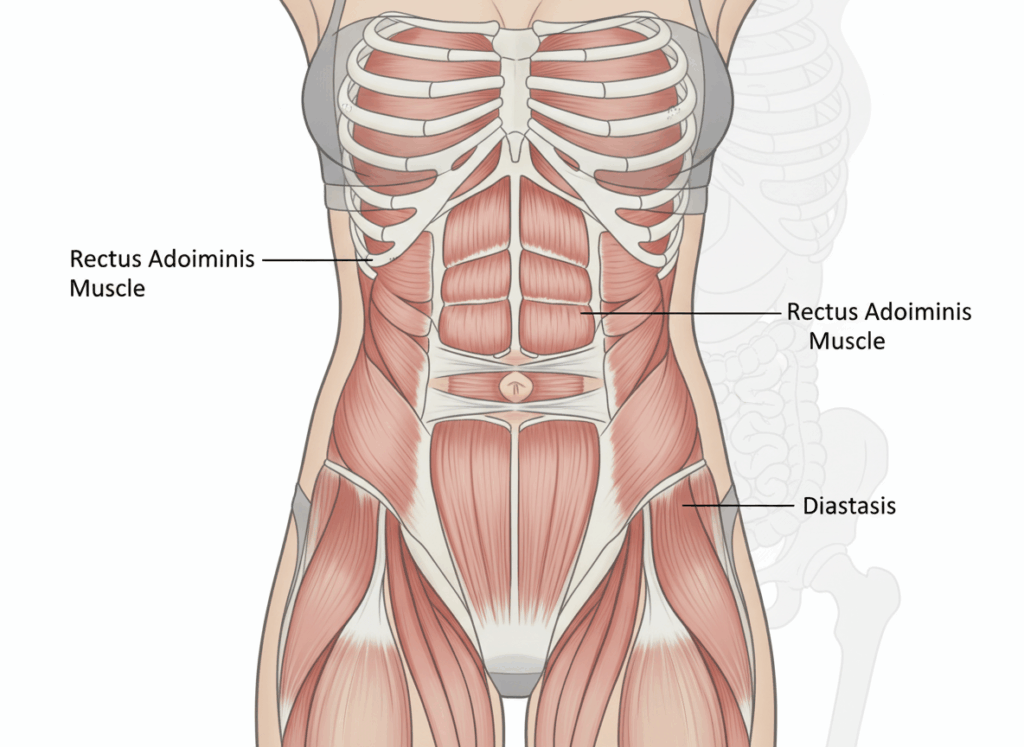
Diastasis recti (DR) is the widening of the space between your rectus abdominis muscles—your “six-pack” muscles—along the linea alba, the connective tissue that runs down the center of your abdomen. Some degree of separation is completely normal and necessary during pregnancy. Your body literally needs to make room for a growing baby.
The issue isn’t the separation itself—it’s whether your core can generate functional tension and manage intra-abdominal pressure effectively after birth. This is an important distinction that gets lost in most discussions about DR.
What causes it:
- Pregnancy (the primary cause—66% of women in their third trimester have some degree of DR)
- Hormonal changes that soften connective tissue
- Pressure from growing uterus pushing abdominal muscles apart
- Multiple pregnancies
- Large babies or multiples
- Genetic factors affecting connective tissue quality
What it looks like:
- A visible ridge or bulge down the center of your abdomen when you engage your core
- Dome-shaped appearance when doing exercises like crunches
- Gap you can feel between your abdominal muscles
- Sometimes accompanied by lower back pain or pelvic floor dysfunction
The Self-Assessment (And Its Limitations)
You can check yourself for DR at home, but understand this is a screening, not a diagnosis:
How to check:
- Lie on your back with knees bent, feet flat
- Place fingers horizontally just above your belly button
- Lift your head and shoulders slightly (mini crunch position)
- Feel for the gap between your abdominal muscles
- Measure the width in finger-widths
What the measurement means:
- 1-2 finger widths: Normal postpartum separation
- 2-3 finger widths: Moderate diastasis
- 3+ finger widths: Significant diastasis
The critical part everyone misses: Gap width alone doesn’t determine function. What matters more is:
- Can you generate tension in the linea alba (does it feel firm or mushy)?
- Do you see doming or bulging with core engagement?
- Can you manage intra-abdominal pressure during activities?
Current research shows that tissue tension and function matter more than absolute gap width. You can have a 2-finger gap with good tension and excellent function, or a 1-finger gap with poor tension and compromised core strength.
When to see a professional: If you have a gap of 2+ fingers, visible doming, pain, or functional limitations, consult a pelvic floor physical therapist or healthcare provider who specializes in postpartum recovery.
Pilates During Pregnancy: Building Foundation While Growing a Baby
Pilates can be excellent during pregnancy for maintaining core strength, preparing for birth, and potentially reducing DR severity. But modifications are essential.
Before You Start
Get medical clearance. If you have any pregnancy complications (placenta previa, preterm labor risk, preeclampsia, etc.), your healthcare provider may advise against exercise.
Find qualified instruction. Not all Pilates instructors have prenatal training. Look for someone with specific prenatal/postnatal certification who understands pregnancy-related modifications.
Pregnancy-Safe Pilates Principles
Focus on deep core, not superficial abs: Your transverse abdominis (the deep corset muscle) supports your growing belly and helps prevent excessive DR. Exercises that engage this muscle are beneficial.
Avoid supine (lying on back) positions after first trimester: Lying flat can compress your vena cava (major vein), restricting blood flow. Use props to elevate your upper body or switch to side-lying and standing positions.
Skip exercises that cause doming or coning: If you see your abdomen creating a ridge or cone shape during an exercise, stop immediately. This indicates excessive pressure on the linea alba.
Modify as you grow: What works in your first trimester won’t work in your third. Good instructors continually adjust exercises as your body changes.
Include pelvic floor awareness: Pilates breathing naturally coordinates with pelvic floor function. This awareness serves you during labor and postpartum recovery.
Safe Prenatal Pilates Exercises
Breathing with TA engagement: Practice lateral ribcage breathing with gentle transverse abdominis activation. This is foundational.
Side-lying leg series: Strengthens hips and obliques without loading your abdomen.
Modified bridges: Strengthens glutes and posterior chain. Stop if you feel lightheaded.
Cat-cow and pelvic tilts: Mobilizes spine and relieves back tension.
Standing work: Squats, lunges, and standing leg work with core engagement.
Modified planks: From elevated positions (wall, counter) in later pregnancy.
Exercises to Avoid During Pregnancy
Deep forward flexion: Full sit-ups, roll-ups, or exercises that create significant abdominal pressure.
Lying flat on back: After 20 weeks or whenever it feels uncomfortable.
Deep twists: Gentle rotation is fine; deep twisting compresses your abdomen.
Exercises that cause doming: Any movement that creates visible coning along your midline.
Postpartum Pilates: The Smart Recovery Approach
After birth, your approach to Pilates needs to be strategic, progressive, and individualized based on your delivery, DR severity, and healing timeline.
Timing Your Return
Vaginal delivery: Wait for 6-week medical clearance (or longer if complications).
C-section delivery: Wait for 8-12 week clearance minimum. You’ve had major abdominal surgery.
Before clearance: Focus on gentle breathing, pelvic floor awareness (not exercises yet), and basic activities of daily living.
Reassessing Your DR Postpartum
Check again around 6-8 weeks postpartum. Your gap may have narrowed naturally through the healing process, or it may persist. Either way, this assessment helps guide your recovery plan.
If you have significant DR (3+ fingers or poor tissue tension):
- Work with a pelvic floor physical therapist
- Start with very foundational exercises
- Progress slowly based on tissue response
- Avoid traditional ab work until your core can manage it
If you have moderate DR (2-3 fingers with decent tension):
- Begin with modified Pilates focusing on deep core
- Progress based on absence of doming
- Build gradually toward traditional exercises
If minimal separation (1-2 fingers with good tension):
- You can likely progress through standard postpartum Pilates progressions
- Still start conservatively and build up
- Monitor for any doming or dysfunction
The Doming Test: Your Real-Time Feedback
During ANY postpartum exercise, watch your abdomen. If you see:
- A ridge or tent-like shape along your midline
- Doming or bulging outward
- Your belly pushing out instead of drawing in
This means you’re exceeding your tissue’s current capacity. Response: reduce range of motion, decrease resistance, or choose a different exercise. Doming isn’t dangerous, but it indicates you’re not ready for that level of challenge yet.
Pilates Exercises for DR Recovery
These exercises specifically target the deep core system while respecting healing tissue:
Phase 1: Reconnection (Weeks 6-8 Post-Clearance)
Diaphragmatic breathing with TA engagement: Lie on your back (or semi-reclined if more comfortable), knees bent. Breathe deeply into your ribcage, then exhale slowly while gently drawing your lower belly toward your spine. This reconnects your brain to your deep core.
Pelvic tilts: Gently rock your pelvis between neutral and imprint (flattening lower back to floor). Engage your deep core with the movement. Start with small ranges.
Heel slides: One leg at a time, slide your heel away from your body while maintaining core engagement and neutral spine. This challenges your ability to stabilize while your leg moves.
Pelvic floor coordination: Practice gentle pelvic floor lifts coordinated with your exhale. Think “lift and hug” rather than aggressive kegels.
Phase 2: Building Strength (Weeks 8-16)
Modified dead bug: Knees in tabletop, lower one leg toward floor while maintaining neutral spine and engaging core. Watch for doming—if you see it, reduce your range.
Small bridges: Lift hips while engaging glutes and core. Focus on quality over height. Progress to single-leg variations when ready.
Side-lying leg lifts: Strengthen lateral core and hip stabilizers without loading the linea alba directly.
Modified planks: Start from elevated positions (wall, counter, then floor on knees). Progress to full planks only when you can maintain form without doming.
Standing work with core engagement: Squats, lunges, single-leg balance—all with intentional core activation.
Phase 3: Progressive Challenge (Months 4-6+)
Roll-up progressions: Start with bent knees and limited range. Progress to full roll-ups only when your tissue can handle it without doming.
Plank variations: Full planks, side planks, plank with leg lifts—all progressions that require excellent core control.
Traditional Pilates mat repertoire: Hundred, single leg stretch, criss-cross—reintroduce gradually based on your tissue’s response.
Exercises to Continue Avoiding or Modifying
Traditional crunches and sit-ups: These create significant midline pressure and are often contraindicated for DR.
Double leg lowers: High load on core. Single leg variations are safer.
Deep forward flexion: Full roll-ups, teaser—only when your tissue is ready.
Heavy overhead lifting: Creates downward pressure. Build up gradually.
What Actually Helps DR Recovery
Consistent deep core activation: Your transverse abdominis needs to relearn its job. Consistent practice matters more than intensity.
Breath coordination: Proper breathing creates intra-abdominal pressure management, which is essential for core function.
Progressive loading: Gradually increasing challenge as your tissue adapts and strengthens.
Whole-body strength: Your core doesn’t exist in isolation. Hip strength, back strength, and pelvic floor function all contribute.
Patience: Tissue healing and neuromuscular retraining take months, not weeks.
What Doesn’t Actually Help
Abdominal binders or wraps: May provide temporary support or comfort but don’t strengthen tissue or “close the gap.”
Obsessing over gap width: Function matters more than millimeters.
Avoiding all core work: Creates weakness rather than protection. Smart, progressive exercise is therapeutic.
Comparing your timeline to others: Everyone’s tissue, pregnancy experience, and recovery differs.
When Professional Help is Essential
See a pelvic floor physical therapist if you experience:
- Gap wider than 3 fingers at 6+ months postpartum
- Visible doming with basic daily activities
- Lower back or pelvic pain
- Pelvic floor dysfunction (incontinence, prolapse symptoms, pain)
- Uncertainty about exercise safety
- Lack of progress after several months of consistent effort
PT can provide hands-on assessment, personalized exercise prescription, and manual therapy to improve tissue quality and function.
The Realistic Recovery Timeline
Months 1-3 postpartum: Focus on reconnection and foundational work. Gap may still be wide; that’s normal.
Months 3-6: Progressive strengthening. You should see functional improvements even if gap width hasn’t changed dramatically.
Months 6-12: Continued strengthening and returning to more advanced exercises. Most women see significant improvement in this timeframe.
12+ months: Some women’s gaps fully close; others maintain a small gap with excellent function. Both outcomes are successful if you’re pain-free and functional.
Research shows that with appropriate exercise, most women see improvement in DR within 6-12 months. However, “improvement” means better function and tissue tension, not necessarily complete closure.
The Bottom Line
Diastasis recti is common, manageable, and responds well to intelligent exercise. Pilates offers an excellent framework for recovery through its emphasis on deep core engagement, breath coordination, and progressive strengthening.
The keys to success:
- Start with professional assessment
- Progress based on your tissue’s response, not arbitrary timelines
- Watch for doming and adjust accordingly
- Focus on function over gap width
- Be patient with the healing process
- Seek professional help when needed
Your body accomplished something extraordinary by growing and birthing a baby. The separation that occurred was necessary and normal. Give your tissue the time, appropriate exercise, and professional support it needs to recover function and strength.
You don’t need to “close your gap” to have a strong, functional core. You need to rebuild the coordination, strength, and pressure management that allows your core to do its job effectively. Pilates, done intelligently and progressively, helps you achieve exactly that.